The Road Back: Navigating Stem Cell Transplant
Undergoing a stem cell transplant is often compared to climbing a mountain. The preparation and the procedure itself the conditioning chemotherapy and the infusion are the steep ascent. However, any mountaineer will tell you that the descent is just as critical as the climb. In the medical world, this descent is the recovery phase. It is a period defined by patience, vigilance, and gradual healing.
For patients and their families, understanding the timeline of Stem Cell Transplant Recovery and Follow-up is essential for managing expectations. Recovery is not a linear event that happens the moment you leave the hospital; it is a dynamic process that unfolds over months, and sometimes years, as the immune system rebuilds itself from the ground up.
Phase 1: The Immediate Aftermath (Engraftment)
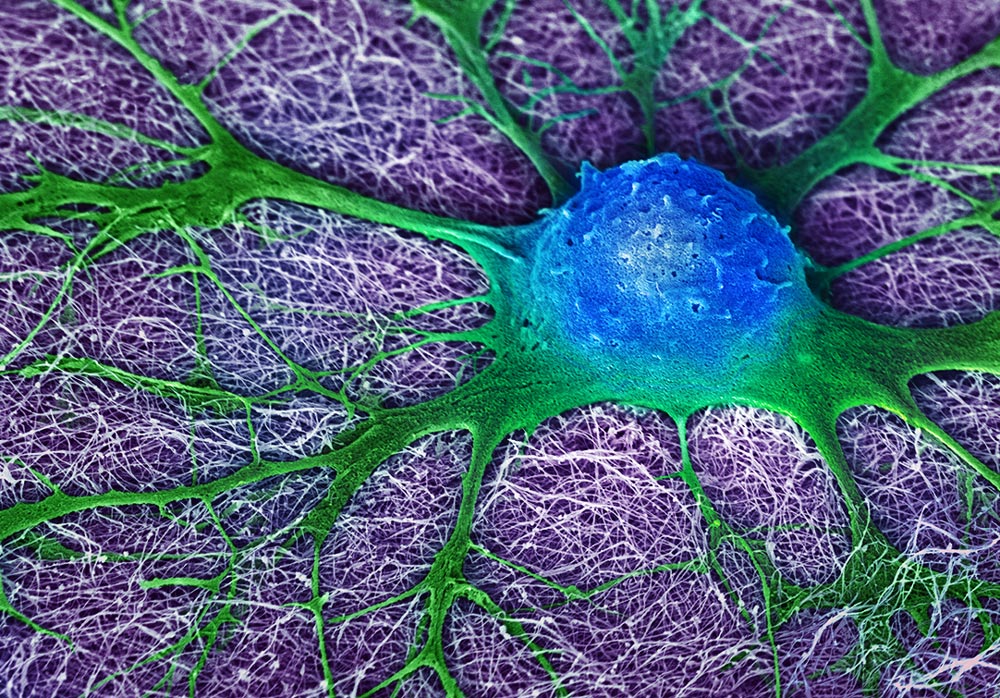
The recovery clock starts ticking the moment the infusion ends. The first milestone is engraftment the point where the transplanted stem cells make their way to the bone marrow and begin producing new blood cells. This typically happens 10 to 28 days after the transplant.
During this window, patients are at their most vulnerable. The body has practically no immune system (neutropenia), meaning a simple bacteria that usually lives harmlessly on the skin could cause a severe infection. This is why the initial recovery usually takes place in a specialized, filtered-air hospital unit.
Patients may experience side effects from the conditioning chemotherapy, such as mucositis (mouth sores), nausea, and fatigue. The medical team’s priority during this phase is supportive care: managing pain, preventing infection with prophylactic antibiotics, and supporting the body with blood or platelet transfusions until the new marrow takes over.
Phase 2: The First 100 Days
Discharge from the hospital is a joyous milestone, but it signals a shift in responsibility. The period extending up to roughly 100 days post-transplant is critical. While the blood counts have recovered enough to leave the hospital, the immune system is still in its infancy comparable to that of a newborn baby.
During this phase, the “new normal” involves strict precautions:
- Infection Control: Frequent hand washing is non-negotiable. Patients are often advised to wear high-filtration masks in public and avoid crowds or sick individuals.
- Dietary Restrictions: Because the gut is still healing, patients may need to follow a “neutropenic diet,” avoiding raw foods, unpasteurized dairy, and undercooked meats to reduce the risk of foodborne illness.
- Environmental Safety: Activities like gardening or cleaning litter boxes are generally prohibited due to the risk of fungal infections (like Aspergillus or Toxoplasmosis) found in soil and animal waste.
Watchful Waiting: GVHD and Complications
For patients who have undergone an allogeneic transplant (using a donor’s cells), a primary focus of follow-up is monitoring for Graft-versus-Host Disease (GVHD). This occurs when the donor’s immune cells perceive the patient’s body as “foreign” and attack it.
GVHD can be acute (occurring in the first few months) or chronic (developing later). Symptoms can vary widely, affecting the skin (rashes), liver (jaundice), or digestive tract (nausea, diarrhea). It is a treatable condition, usually managed with immunosuppressive medications, but early detection is key. This is why follow-up appointments are frequent often weekly or bi-weekly in the early stages.
Long-Term Follow-up and Revaccination
As the months pass, the focus shifts from acute survival to long-term quality of life. By the six-month or one-year mark, if the immune system has recovered sufficiently, the medical team will begin a revaccination program. Since the transplant wipes out previous immune memory, patients often need to be re-immunized against childhood diseases like measles, mumps, and polio.
At Liv Hospital, our commitment to patient care extends well beyond the procedure room. We understand that survivorship involves monitoring for late effects of chemotherapy, such as hormonal changes, bone density issues, or cardiovascular health. Our multidisciplinary team ensures that every survivor has a structured roadmap for long-term health maintenance, ensuring that the “gift of life” received through the transplant is preserved and protected.
Restoring Balance to Body and Mind
Ideally, full recovery from a stem cell transplant is measured not just by blood counts, but by the return to daily joys work, hobbies, and family life. However, the physical and emotional toll of the journey can linger. Fatigue is a common complaint even months after treatment concludes. It is vital to listen to your body, prioritizing rest and gradual physical rehabilitation. As you navigate this new chapter of survivorship, integrating holistic wellness practices can be incredibly empowering. For tips on nutrition, gentle exercise, and mental well-being to help you live and feel stronger every day, exploring lifestyle-focused resources can be a valuable part of your healing toolkit.