A Critical First Step Toward Treatment
Stem cell transplantation is one of the most advanced and potentially life-saving procedures in modern medicine. It is commonly used in the treatment of serious blood disorders, immune system diseases, and certain types of cancer such as leukemia, lymphoma, and multiple myeloma. While many people focus on the transplant itself, one of the most important stages occurs well before the procedure begins: diagnosis and evaluation.
A stem cell transplant is not a standard treatment for every patient. Because it is complex and involves significant risks, a thorough medical evaluation is essential to determine whether a transplant is appropriate, safe, and likely to succeed. At specialized centers such as Liv Hospital, transplant teams use advanced diagnostic tools and multidisciplinary expertise to carefully assess each patient before moving forward.
Why Diagnosis and Evaluation Matter Before a Stem Cell Transplant
Stem cell transplantation works by replacing damaged or diseased bone marrow with healthy stem cells capable of producing normal blood cells. However, the process requires intensive chemotherapy or radiation therapy beforehand, which temporarily weakens the immune system and places stress on multiple organs.
For these reasons, physicians must answer several key questions before recommending a transplant:
- What is the exact diagnosis and disease stage?
- Is the patient medically fit for intensive treatment?
- What type of transplant is most suitable?
- Is there a compatible stem cell donor available?
- What risks or complications should be anticipated?
A detailed evaluation helps ensure the best possible outcome and reduces the likelihood of serious complications.
Conditions That May Require Stem Cell Transplantation
Stem cell transplants are most often used for disorders that affect blood cell production or immune function. These include:
- Acute and chronic leukemias
- Hodgkin and non-Hodgkin lymphoma
- Multiple myeloma
- Severe aplastic anemia
- Myelodysplastic syndromes (MDS)
- Certain inherited immune deficiencies
Each condition has specific criteria that determine whether transplant is recommended, and evaluation is tailored accordingly.
Step One: Confirming the Diagnosis
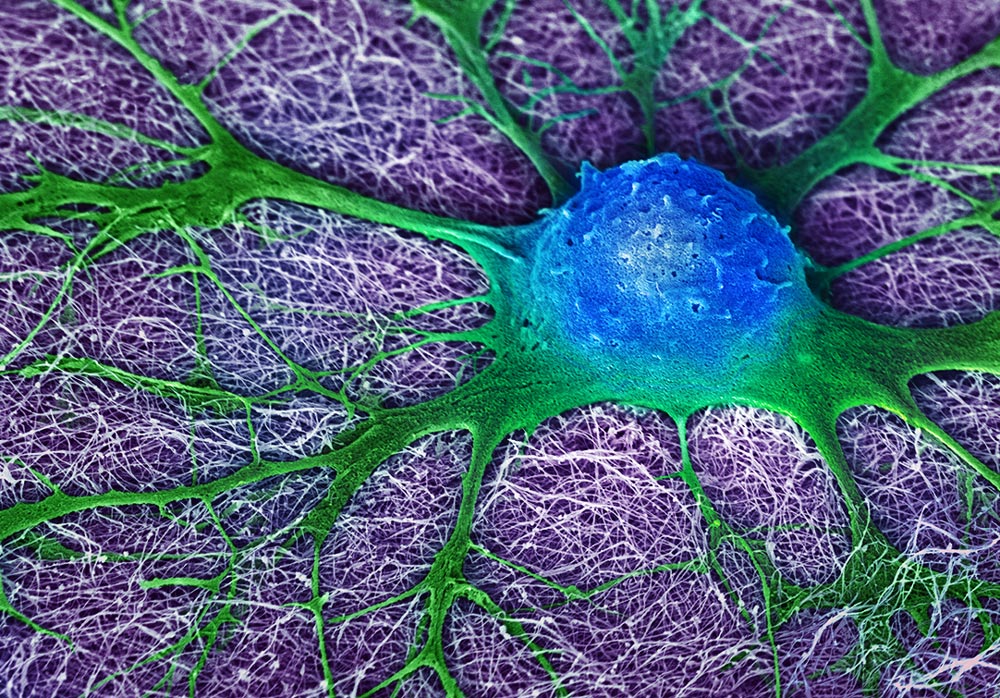
The transplant process begins with confirming the underlying disease through comprehensive diagnostic testing. Common evaluations include:
Blood Tests
A complete blood count (CBC) measures red cells, white cells, and platelets. Abnormal levels can indicate bone marrow dysfunction or malignancy.
Bone Marrow Aspiration and Biopsy
This is one of the most critical diagnostic procedures. A sample of bone marrow is examined to determine:
- Presence of cancerous or abnormal cells
- Disease severity
- Response to previous treatments
Genetic and Molecular Testing
Many blood cancers require chromosomal or mutation testing to assess prognosis and guide treatment planning. Certain genetic markers may influence transplant timing and approach.
Step Two: Assessing Transplant Eligibility
Once diagnosis is confirmed, physicians evaluate whether the patient is a suitable candidate. This involves a complete medical assessment of overall health.
Key Factors Considered Include:
- Age and functional status
- Disease progression and treatment history
- Existing medical conditions (diabetes, heart disease, lung disease)
- Organ function and physical resilience
Stem cell transplantation is intensive, so patients must be able to tolerate both the conditioning therapy and the recovery process.
Organ Function Testing Before Transplant
A major part of evaluation involves ensuring that vital organs can handle the procedure.
Heart Evaluation
Tests such as echocardiograms or ECGs are performed to confirm healthy cardiac function.
Lung Function Testing
Pulmonary function tests measure breathing capacity, especially important because infections and inflammation can occur post-transplant.
Liver and Kidney Function Tests
The liver and kidneys play essential roles in processing chemotherapy drugs and eliminating toxins. Poor function may increase transplant risks.
Infectious Disease Screening
Because transplant patients experience immune suppression, infection prevention is critical. Before transplantation, patients are screened for viruses and infections such as:
- Hepatitis B and C
- HIV
- Cytomegalovirus (CMV)
- Epstein-Barr virus (EBV)
Vaccination history is also reviewed, and preventive treatment plans are established.
Donor Matching and Stem Cell Source Evaluation
For allogeneic transplants (donor stem cells), donor selection is one of the most important steps.
HLA Typing
Human leukocyte antigen (HLA) testing determines tissue compatibility between patient and donor. A close match reduces the risk of complications such as graft-versus-host disease (GVHD).
Stem Cell Sources
Stem cells may come from:
- Bone marrow
- Peripheral blood
- Umbilical cord blood
The transplant team selects the best source depending on disease type and donor availability.
Psychological and Support System Assessment
A stem cell transplant is not only physically demanding but emotionally challenging. Most centers evaluate:
- Mental health readiness
- Stress and coping ability
- Family or caregiver support
- Ability to follow long-term follow-up care
Strong social support plays a major role in recovery success.
Personalized Treatment Planning
After completing diagnostic testing and eligibility evaluation, the transplant team develops a customized plan that includes:
- Type of transplant (autologous vs. allogeneic)
- Conditioning therapy approach
- Infection prevention strategy
- Expected recovery timeline
- Long-term follow-up schedule
For more detailed clinical information, patients can explore Stem Cell Transplant Diagnosis and Evaluation, which outlines the full process and medical standards involved.
Moving Forward With Confidence
Diagnosis and evaluation are the foundation of a successful stem cell transplant journey. This careful process ensures that transplantation is the right option, identifies potential risks early, and allows physicians to design the safest and most effective treatment strategy.
With expert medical teams, advanced technology, and comprehensive patient-centered care, institutions like Liv Hospital help patients approach stem cell transplantation with greater clarity and confidence.
As patients prepare for treatment, overall wellness and lifestyle habits can also support recovery and resilience. For additional inspiration on healthy living and balance during the healing journey, you may also explore resources from live and feel.