Deciding Factors for Stem Cell Transplant Conditions and Indications
In the complex world of hematology and oncology, few treatments are as transformative as hematopoietic stem cell transplantation (HSCT). For decades, this procedure commonly known as a bone marrow transplant has served as a critical lifeline for patients facing life-threatening blood disorders. However, it is not a universal cure-all; it is a highly specialized procedure reserved for specific medical scenarios where the potential benefits outweigh the significant risks.
Understanding the specific Stem Cell Transplant Conditions and Indications is vital for patients and caregivers navigating a diagnosis. It helps answer the fundamental question: Why is this aggressive treatment necessary, and who is it for?
The Rationale: Why Transplants are Performed
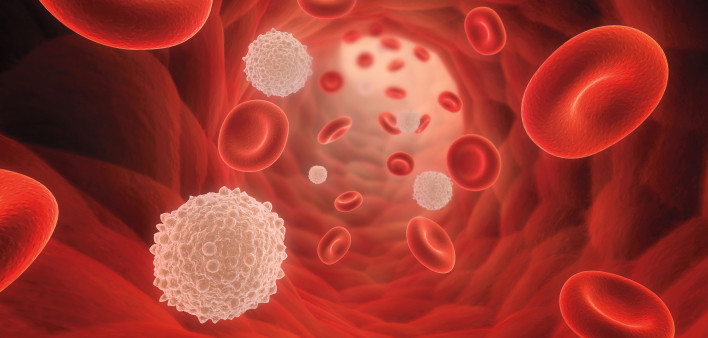
At its core, a stem cell transplant is designed to rescue the bone marrow. The bone marrow is the body’s factory for blood cells, producing red blood cells, white blood cells, and platelets. When this factory is corrupted by cancer, genetic errors, or autoimmune attacks, the consequences are often fatal.
The transplant serves two primary functions depending on the disease:
- Replacement: It allows doctors to use extremely high doses of chemotherapy or radiation to kill cancer cells doses so high they permanently destroy the bone marrow. The transplant then “rescues” the patient by providing new stem cells to rebuild the system.
- Immunotherapy: In the case of donor (allogeneic) transplants, the new immune system recognizes the patient’s remaining cancer cells as foreign and attacks them. This is known as the “graft-versus-tumor” effect.
Malignant Indications: Treating Blood Cancers
The most common reasons for stem cell transplants are malignant diseases affecting the blood and lymphatic systems.
1. Leukemias Leukemia is a cancer of the body’s blood-forming tissues. Transplants are frequently considered for:
- Acute Myeloid Leukemia (AML): Often recommended for patients with high-risk genetic features or those who relapse after initial chemotherapy.
- Acute Lymphoblastic Leukemia (ALL): Common in children and adults; transplants are used when the disease is aggressive or unresponsive to standard treatments.
- Chronic Myeloid Leukemia (CML): While targeted oral therapies (TKIs) are now the first line of defense, transplants remain a curative option for resistant cases.
2. Lymphomas Lymphomas affect the lymphatic system.
- Non-Hodgkin Lymphoma (NHL) & Hodgkin Lymphoma: Autologous transplants (using the patient’s own cells) are a standard of care for patients who have relapsed after initial treatment. It essentially resets the bone marrow after high-dose chemotherapy.
3. Multiple Myeloma This is a cancer of plasma cells. While a transplant is rarely curative for myeloma, it is a standard part of treatment to significantly prolong survival and extend the period of remission (disease-free living).
Non-Malignant Indications: Benign but Critical
It is a misconception that transplants are only for cancer. Several non-malignant conditions, which can be just as life-threatening, are treated and often cured via transplantation.
1. Bone Marrow Failure Syndromes Conditions like Severe Aplastic Anemia occur when the marrow simply stops producing enough blood cells. For younger patients with a matched sibling donor, a transplant is often the treatment of choice.
2. Hemoglobinopathies These are genetic disorders affecting the shape or function of red blood cells.
- Thalassemia Major: Patients rely on lifelong blood transfusions, which cause iron overload. A transplant offers the only potential cure.
- Sickle Cell Disease: Transplants can cure the condition, preventing the severe pain crises and organ damage associated with the disease.
3. Primary Immune Deficiencies For conditions like Severe Combined Immunodeficiency (SCID), often called “bubble boy disease,” a transplant is essential to provide the child with a functioning immune system.
Patient Eligibility: The Assessment Phase
A diagnosis alone does not automatically qualify a patient for a transplant. The decision is multifaceted. Medical teams must evaluate the “biological age” of the patient meaning their overall physical fitness and organ function (heart, lungs, kidneys, and liver).
At Liv Hospital, we utilize a rigorous screening process to ensure patient safety. Our hematology specialists review not just the disease status, but the patient’s overall resilience. Because the conditioning regimens (chemotherapy/radiation) are physically demanding, ensuring the patient can withstand the process is as important as matching the donor.
Moving Forward with Confidence
A stem cell transplant is a major medical intervention that marks a turning point in a patient’s life. It bridges the gap between a life-threatening condition and the possibility of a cure or long-term management. While the medical journey focuses on eradicating disease, the ultimate goal is a return to a vibrant, functional life. As you or your loved ones move through recovery, maintaining a holistic perspective on health becomes a priority. For guidance on nutrition, mental wellness, and restoring balance after treatment, you can explore our dedicated lifestyle resources at live and feel.