Renewing Life at the Cellular Level with Stem Cell Transplants
In the landscape of modern medicine, few treatments are as complex or as potentially life-saving as the stem cell transplant. Often heard in the context of cancer treatment, this procedure represents a profound “reset” for the human body’s blood-forming systems. While the medical terminology can be daunting, understanding the mechanics of this therapy is the first step toward navigating a diagnosis with confidence and clarity.
For patients and families facing a diagnosis of leukemia, lymphoma, or other blood disorders, a Stem Cell Transplant Overview and Definition provides the essential roadmap for what lies ahead. This procedure is not merely a single surgery, but a multi-stage therapeutic journey designed to replace unhealthy bone marrow with healthy, functioning stem cells.
What Exactly is a Stem Cell Transplant?
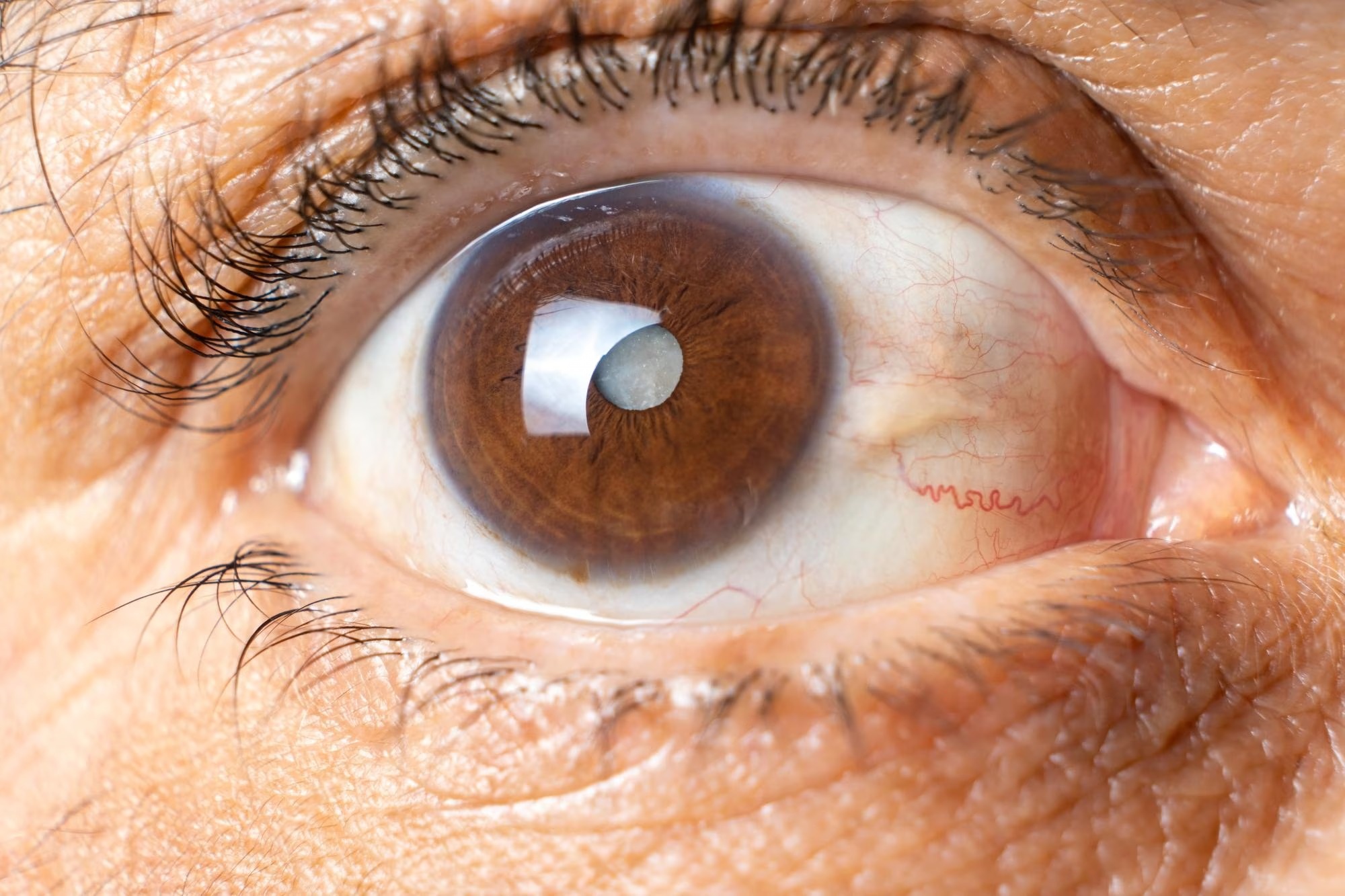
To understand the transplant, we must first understand the “seed.” Stem cells specifically hematopoietic stem cells—are immature cells found in the bone marrow (the soft, spongy center of the bones) and peripheral blood. They are unique because they have the ability to develop into the three essential types of blood cells our bodies need to survive:
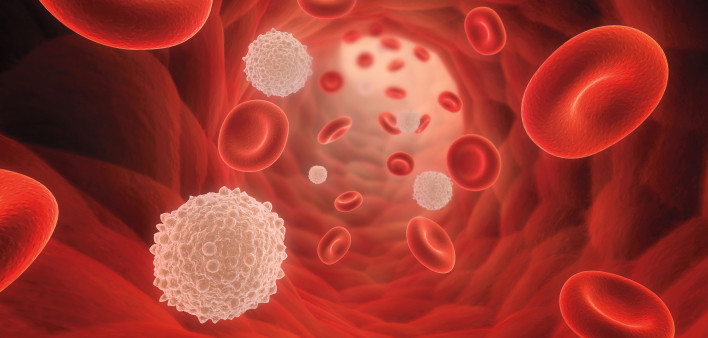
- Red blood cells: Which carry oxygen throughout the body.
- White blood cells: Which fight infection and anchor the immune system.
- Platelets: Which help the blood clot to stop bleeding.
In conditions like leukemia or multiple myeloma, the bone marrow malfunctions, producing excessive or defective cells. A stem cell transplant (sometimes referred to as a bone marrow transplant) involves destroying the diseased marrow with high-dose chemotherapy and/or radiation and then infusing healthy stem cells into the body. These new cells travel to the bone marrow, settle in, and begin the vital work of producing healthy blood cells a process known as engraftment.
The Different Types of Transplants
Not all transplants are the same; the type recommended by a physician depends entirely on the specific disease, the patient’s age, and their overall health stability.
1. Autologous Transplant (Self-Donor) In this procedure, the patient’s own stem cells are collected (harvested) from their blood or bone marrow before they undergo high-dose chemotherapy. The cells are frozen and stored. After the intense treatment eliminates the cancer cells, the stored stem cells are thawed and infused back into the patient. This is commonly used for lymphomas and multiple myeloma. The primary advantage here is that there is no risk of the body rejecting the cells, as they are the patient’s own.
2. Allogeneic Transplant (Donor) Here, the stem cells come from a donor. This donor could be a sibling, an unrelated volunteer found through a registry, or sometimes a parent or child. The key is that the donor’s tissue type (HLA) must closely match the patient’s. Allogeneic transplants have a unique benefit called the “graft-versus-tumor” effect, where the donor’s healthy immune cells recognize and attack any remaining cancer cells in the patient.
3. Syngeneic and Haploidentical Transplants A syngeneic transplant uses cells from an identical twin (a perfect genetic match). A haploidentical transplant uses a “half-matched” donor, typically a parent or child, expanding the possibility of treatment for those who cannot find a full match.
Why Is It Performed?
Stem cell transplants are primarily used when the bone marrow has been destroyed by disease or when it needs to be cleared out to treat an aggressive cancer. Common indications include:
- Acute and Chronic Leukemias (AML, ALL, CML, CLL)
- Hodgkin and Non-Hodgkin Lymphoma
- Multiple Myeloma
- Aplastic Anemia (bone marrow failure)
- Severe Combined Immunodeficiency (SCID)
- Hemoglobinopathies (like Thalassemia or Sickle Cell Disease)
The Transplant Process: A Journey of Resilience
A stem cell transplant is a marathon, not a sprint. The process begins with conditioning, where the patient receives high doses of chemotherapy or radiation. This serves two purposes: to kill cancer cells and to suppress the immune system so it won’t reject the new cells (in allogeneic cases).
Following conditioning is the infusion day often celebrated as a “rebirth day” by survivors. The stem cells are infused through a central line, much like a blood transfusion. It is painless and typically takes a few hours.
The weeks following infusion are critical. Patients stay in protective isolation to prevent infection while waiting for engraftment. During this time, the medical team closely monitors blood counts and manages side effects. At Liv Hospital, our multidisciplinary teams comprising hematologists, oncologists, and infectious disease specialists work in unison to manage these complex phases, ensuring that every patient receives world-class medical surveillance and compassionate care during their most vulnerable moments.
Life After Transplant
Recovery from a stem cell transplant takes time. It involves slowly rebuilding the immune system and regaining physical strength. While the medical aspect is paramount, the journey to full recovery is also deeply personal and holistic. It requires patience, mental resilience, and a focus on overall well-being. As you transition from patient to survivor, integrating healthy habits becomes essential. For insights on how to nurture your body and mind during recovery and beyond, you can explore resources on how to live and feel your best every day.